Regarding the treatment
1. Basic Knowledge about Dialysis
Dialysis is a treatment for end-stage renal failure.
■ Hemodialysis (HD)
Blood is taken out of the body, purified by passing it through an artificial membrane to remove waste products and unnecessary fluids, and then returned to the body.
■ Hemofiltration (HF)
It uses a filtration device with the same mechanism as a dialyzer (artificial membrane) to remove fluids containing waste products and electrolytes.
■ Hemodiafiltration (HDF)
A method that combines both hemodialysis and hemofiltration. This treatment incorporates the advantages of both methods. It removes larger harmful substances than hemodialysis and smaller harmful substances than hemofiltration.
■ Home Hemodialysis (HHD)
To undergo home hemodialysis, it is a mandatory requirement to receive it under the guidance and management of a medical institution. Both the patient and the assistant apply for home hemodialysis at the guiding medical institution.
The medical institution provides explanations such as “To prevent accidents, always follow the manual procedures without skipping any steps” and “If any abnormalities in health or the dialysis equipment occur, it is obligatory to promptly report to the guiding medical institution.”
A decision is then made on whether or not the patient can safely undergo home hemodialysis.
Training prior to introducing home hemodialysis is intensively undertaken for a fixed period (about one month). Subsequently, guidance is provided during regular dialysis times, totaling to around 3 to 5 months of instruction. The guidance includes procedures for dialysis, operation of equipment, handling of abnormal situations, and how to contact the medical institution. This instruction must also be received by the assistant.
<Costs Associated with Home Hemodialysis>
Even at home, insurance is applied in the same way as it is for outpatient treatment, so the out-of-pocket cost remains the same. The dialysis equipment is loaned from the medical institution. Expenses for home modifications to accommodate the dialysis equipment and accessories, purchasing a bed for dialysis, as well as the cost of electricity and water (20,000 – 40,000 yen) used during dialysis, are borne by the patient.
■ Peritoneal Dialysis
This can be done at home. CAPD (Continuous Ambulatory Peritoneal Dialysis) involves changing the dialysis fluid bag several times during the day. It uses the patient’s own peritoneal membrane inside their body to purify the blood. After starting dialysis, it’s suggested that the residual kidney function can be maintained for a longer period than with hemodialysis, possibly delaying the onset of anuria (absence of urine). Clinic visits are typically required about once or twice a month.
○ While hemodialysis is primarily an outpatient treatment (except for HHD), peritoneal dialysis is a home-based treatment. However, you need to visit the clinic approximately twice a month.
○ The duration of hemodialysis is typically 4 to 6 hours per session, three times a week. Some medical facilities offer overnight sessions, making it possible for patients to continue working while undergoing dialysis.
Nowadays, there are various patterns of dialysis treatment available, allowing it to be integrated into the individual’s lifestyle.
2,Survey of Dialysis Patients in Japan
It is estimated that there are approximately 320,000 dialysis patients in Japan. The breakdown is as follows:
Number of Dialysis Patients
- Daytime Hemodialysis: 83.7% (263,109 people)
- Nighttime Hemodialysis: 13.2% (41,365 people)
- Home Hemodialysis: 0.1% (461 people)
- Peritoneal Dialysis: 2.9%
Dialysis History
- 5 to less than 10 years: 25.1%
- 10 to less than 15 years: 12.9%
- 15 to less than 20 years: 6.8%
- Over 20 years: 7.9%
- The longest recorded dialysis history is 45 years and 7 months
(as of the end of December 2013).
3, Causes of Malaise After Dialysis and Improvement Methods
Depending on the type of dialysis, the causes of malaise and the methods of improvement vary. It is essential to adjust to ensure an adequate amount of dialysis within one’s lifestyle. It’s also vital to consider any complications or other underlying illnesses.
4,Reasons for Reduced Urine Output after Starting Dialysis
Dialysis is started because of a disease called chronic renal failure. The kidneys are almost non-functional, so they cannot produce urine and, simultaneously, cannot expel toxins from the body.
Therefore, dialysis is used to collect and expel these toxins from the body. As dialysis takes over the function of the kidneys, the kidneys eventually become redundant. An organ that is no longer used will gradually atrophy.
Hence, as dialysis continues, most patients become anuric. Even if urine is produced, it does not sufficiently expel the body’s toxins, so dialysis remains necessary.
5,Is Dietary Restriction Necessary After Dialysis?
Indeed, the strict dietary restrictions required before starting dialysis might be reduced, and more foods may become permissible. However, since urine output may decrease, salt restrictions and dietary controls to prevent complications remain essential.
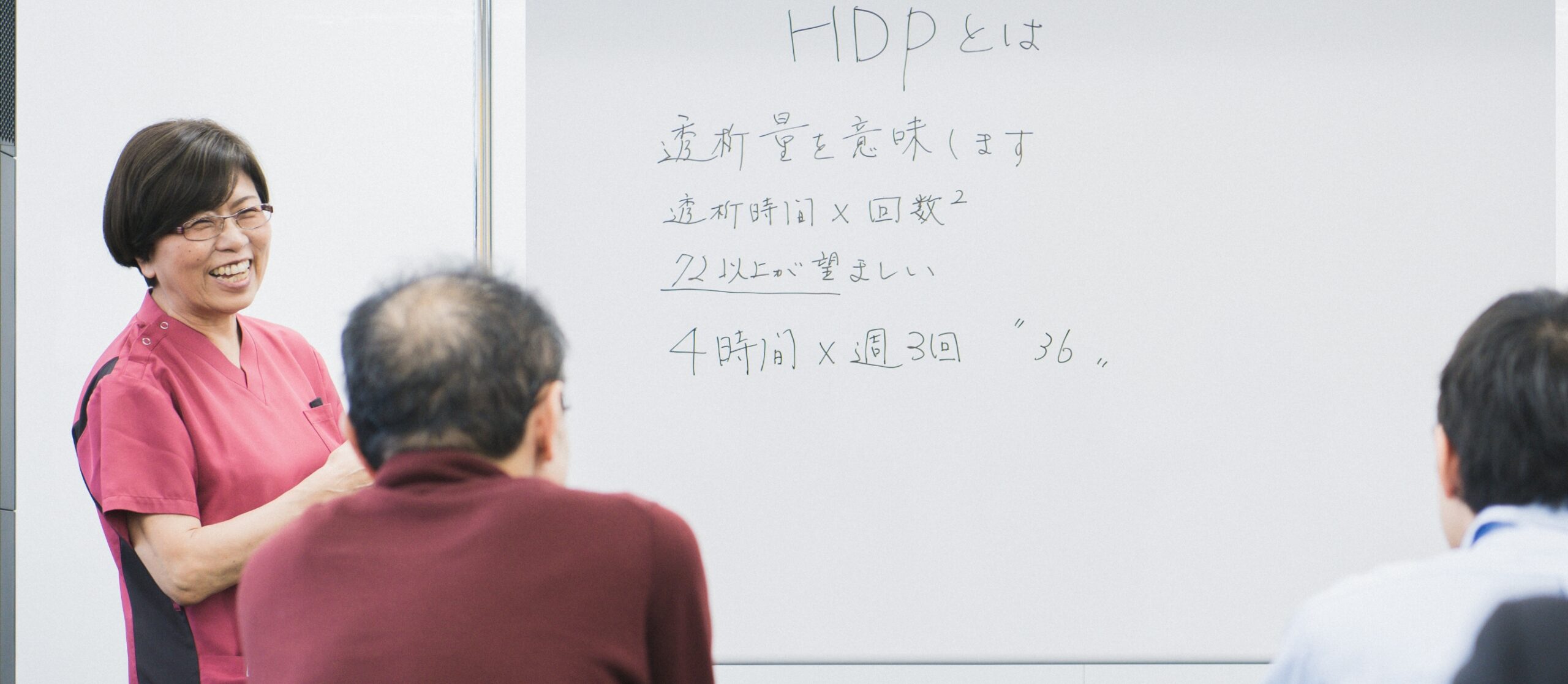
6,Extending Dialysis Time is Beneficial for Life Expectancy
Current artificial kidneys and related equipment have vastly improved compared to their initial stages. Reports suggest that the longer the dialysis, the better the life prognosis. Considering individual work and lifestyle, striving for a longer dialysis time is crucial.
7,Ways to Alleviate Irritability During Dialysis
It’s common to feel irritable during dialysis, possibly due to an accumulation of uremic toxins in the body because of insufficient dialysis. First, consider extending the dialysis time. If that’s difficult, try increasing the dialysis amount by enlarging the dialyzer volume or raising the blood flow rate during dialysis.
8,Criteria for Determining Dry Weight in Dialysis Patients
In people with normal kidney function, excess water is expelled in urine, so the value shown on the scale directly corresponds to their actual weight. However, for dialysis patients who produce little to no urine, the weight can vary significantly before and after dialysis, making it hard to ascertain the actual body weight.
It’s crucial to weigh oneself to determine if excess water from the body has been adequately expelled. Therefore, the proportion of the heart to the thoracic cavity (cardiothoracic ratio) is determined from chest X-ray images of dialysis patients. The target ratio is below 50%. Considering any blood pressure drops during dialysis and heart function status evident from blood tests, a tentative weight is determined. This weight is referred to as the “dry weight.”
This value serves as a target for adjusting dialysis to extract excess water from the body, making the dry weight the goal weight for dialysis.
Actual body weight can vary with diet, physical condition, etc. Nevertheless, neglecting regular measurement of dry weight can lead to water retention and the potential onset of heart failure.
If your physician does not regularly measure dry weight, consider requesting a review of your dry weight whenever changes in your physical condition or food intake are observed.
